Agentic AI in Healthcare
Provide intelligent guidance that empowers members to understand their benefits with ease
With any health insurance, you expect a clear understanding of your medical and drug coverage, out of pocket expenses and your in-network provider availability.
Unfortunately, that is not the experience for MVP members.
- Members have to either call in, wait on hold and rely on verbal confirmations and quotes
- Or members need to navigate online, search through large PDF documents, decode complex industry terminology and healthcare acronyms, and then assume the risk of misunderstanding their coverage.
Discovering this pain point, MVP looked to build their first in-house, agentic LLM that would allow members to self-service their benefit coverage.
Impact
- Researched 100+ member pain points, established UX x AI principles, helped build evaluation guide, and design final prototype
- Launched a prototype AI to the 1500+ MVP employees for testing and feedback
Role
Team
- 1 Product Manager
- AI Council
- 2 Tech Teams
- 1 Designer
Time
skills
DISCOVER
Objective
Understand what are the main pain points and challenges for members in interpreting benefits, finding care and reading the formulary
Contribution
Worked directly with 5 call center staff to document pain points, pulled analytics on frequent customer contact reasons, and defined UX problem scope for AI solution development
Result
Co-synthesized problem space, opportunities and risk considerations into a presentation for leadership. Idea was pushed to AI council, receiving green-light
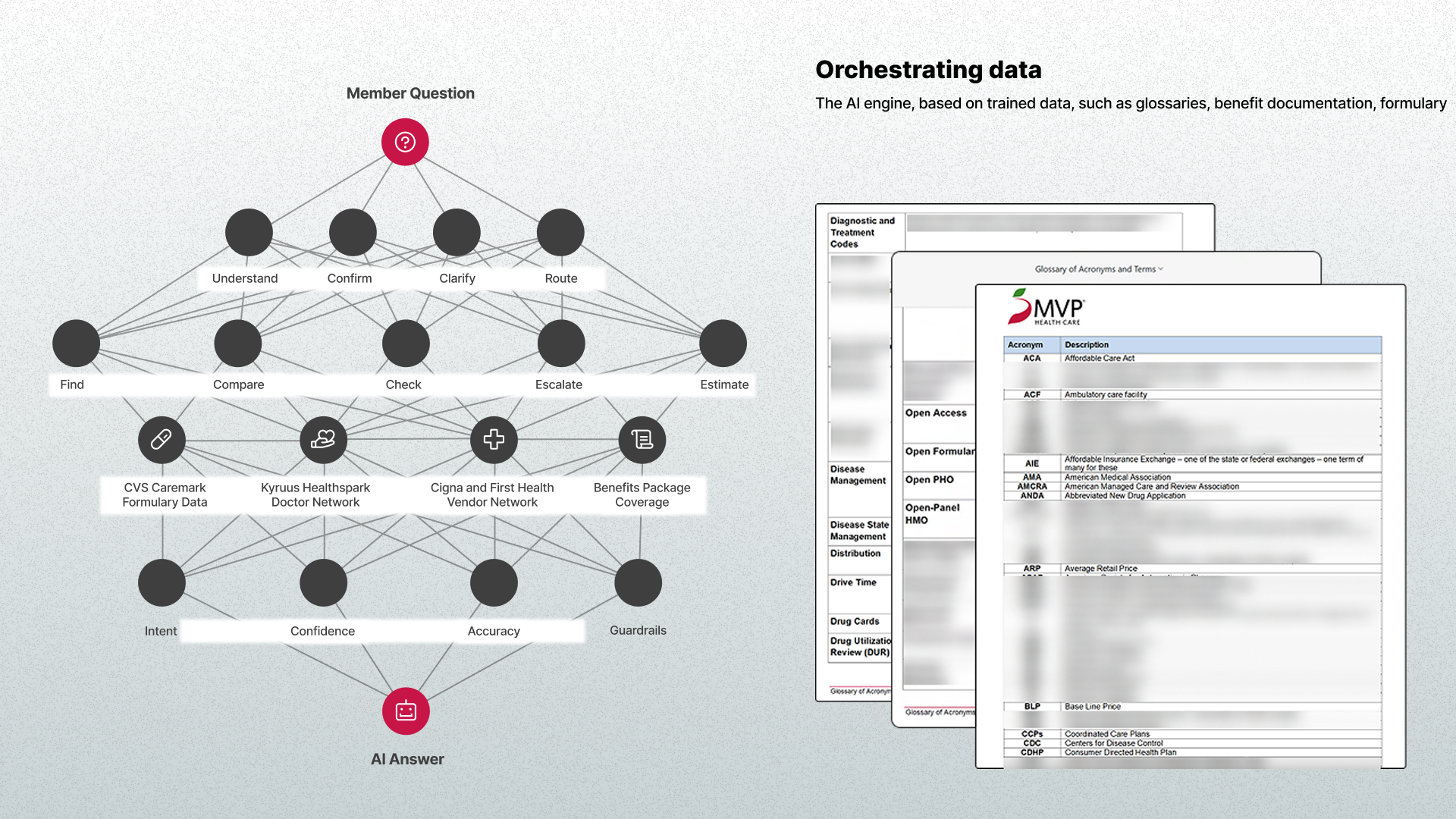
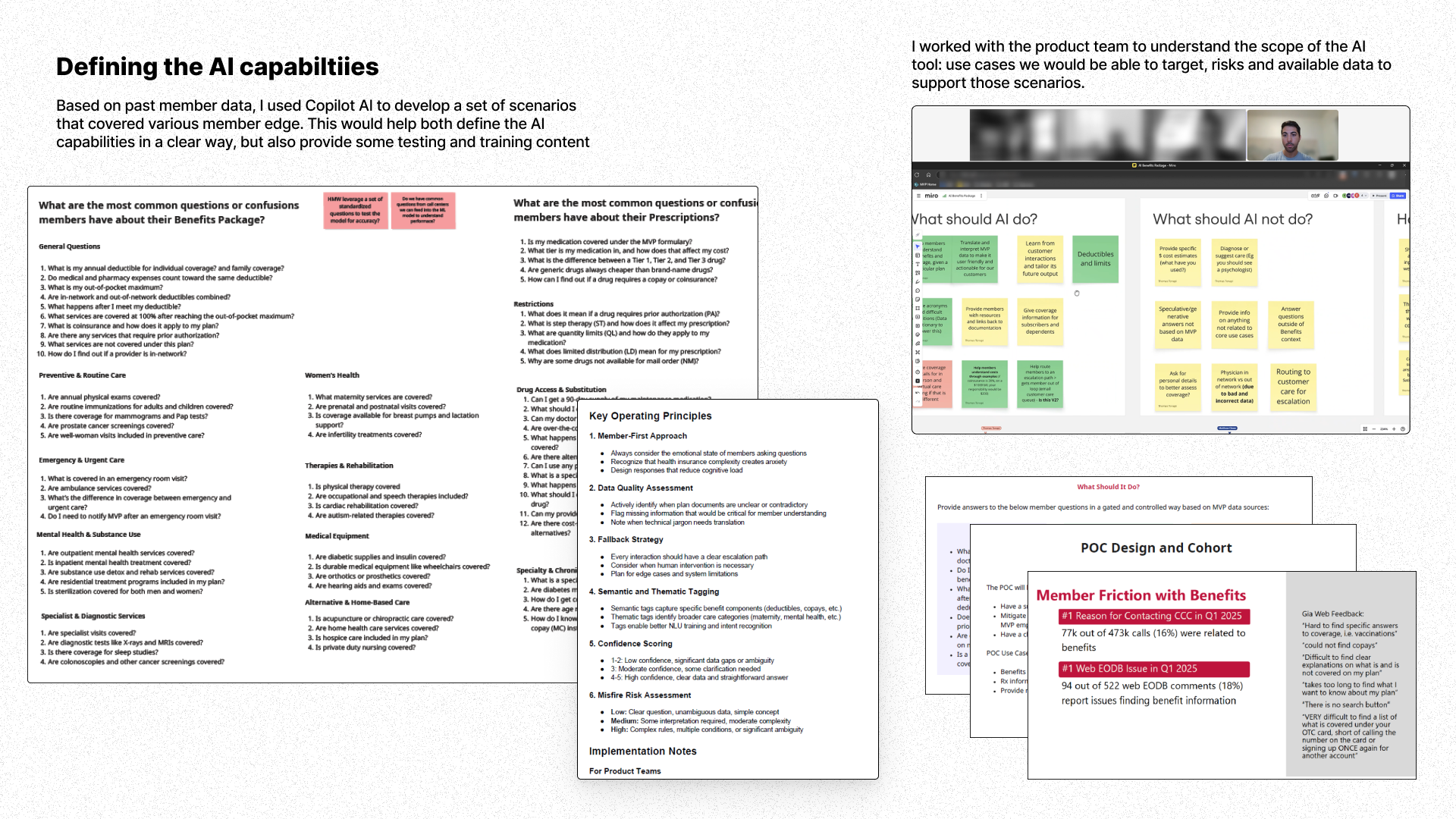
Define
Objective
Pull data and APIs, tag and normalize data. For UX, set boundaries for the LLM and assist in defining testing cases
Contribution
Developed a set of 50+ scenarios and questions, defined conversational principles and helped validate a grounding glossary of 280+ healthcare terms
Result
Engineers were able to successfully parse PDFs, spreadsheets and pull API data. Integrate UX considerations like tone, escalation path, actionability into model parameters
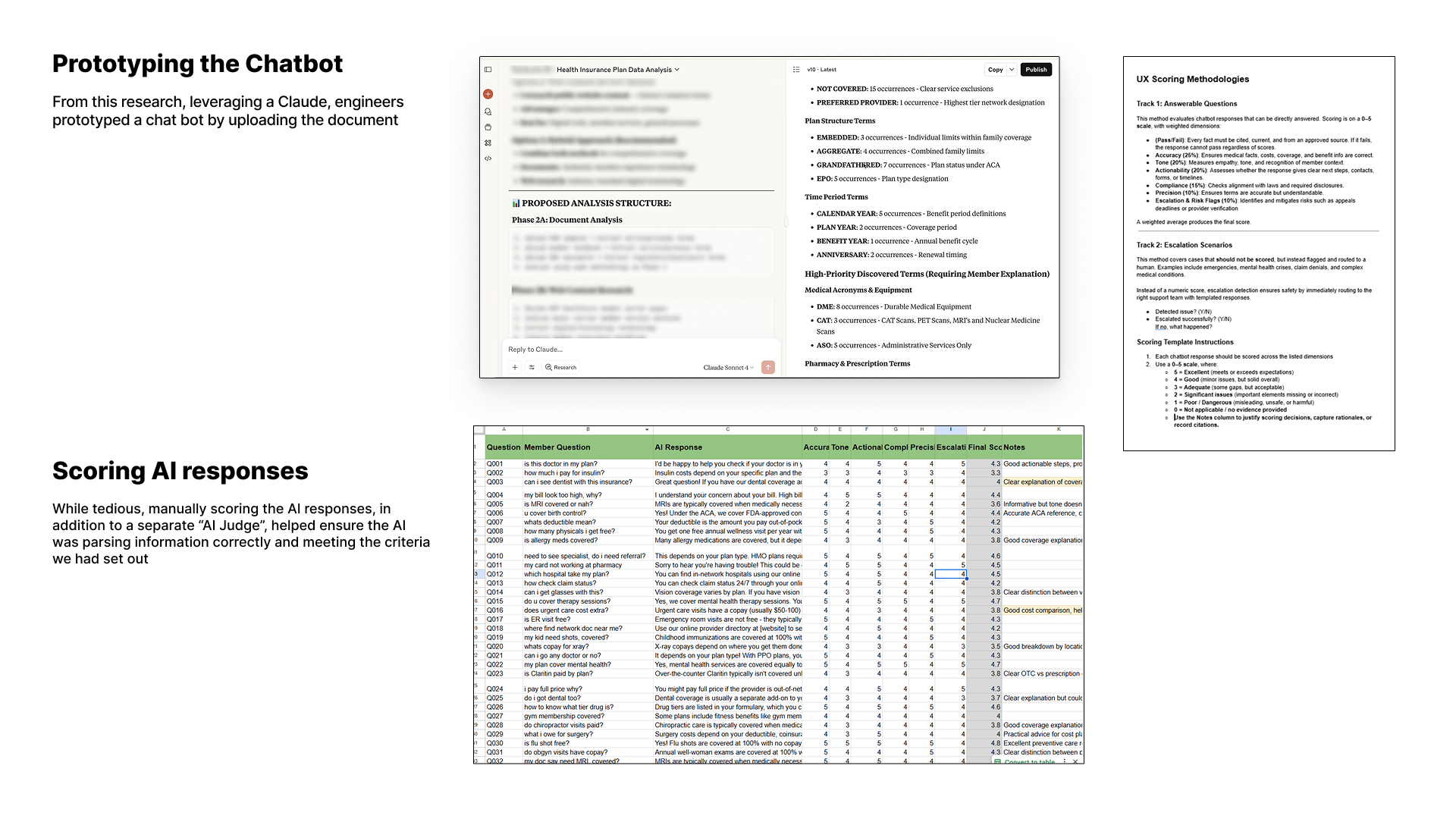
Design
Objective
Begin testing prototype in Claude Opus, ranking responses and validate outputs are in line with problem statement
Contribution
Worked to build a UX success measurement plan. Collaborated with customer care to pull a sample of ~500 questions from member chats for evaluation. Co-prepared scoring guide and walkthrough with 5 agents
Result
Call center agents provided AI response feedback, allowing engineers to fine tune the model
Synthesize
Objective
Create an entry point for the AI assistant within MVP’s existing member portal experience
Contribution
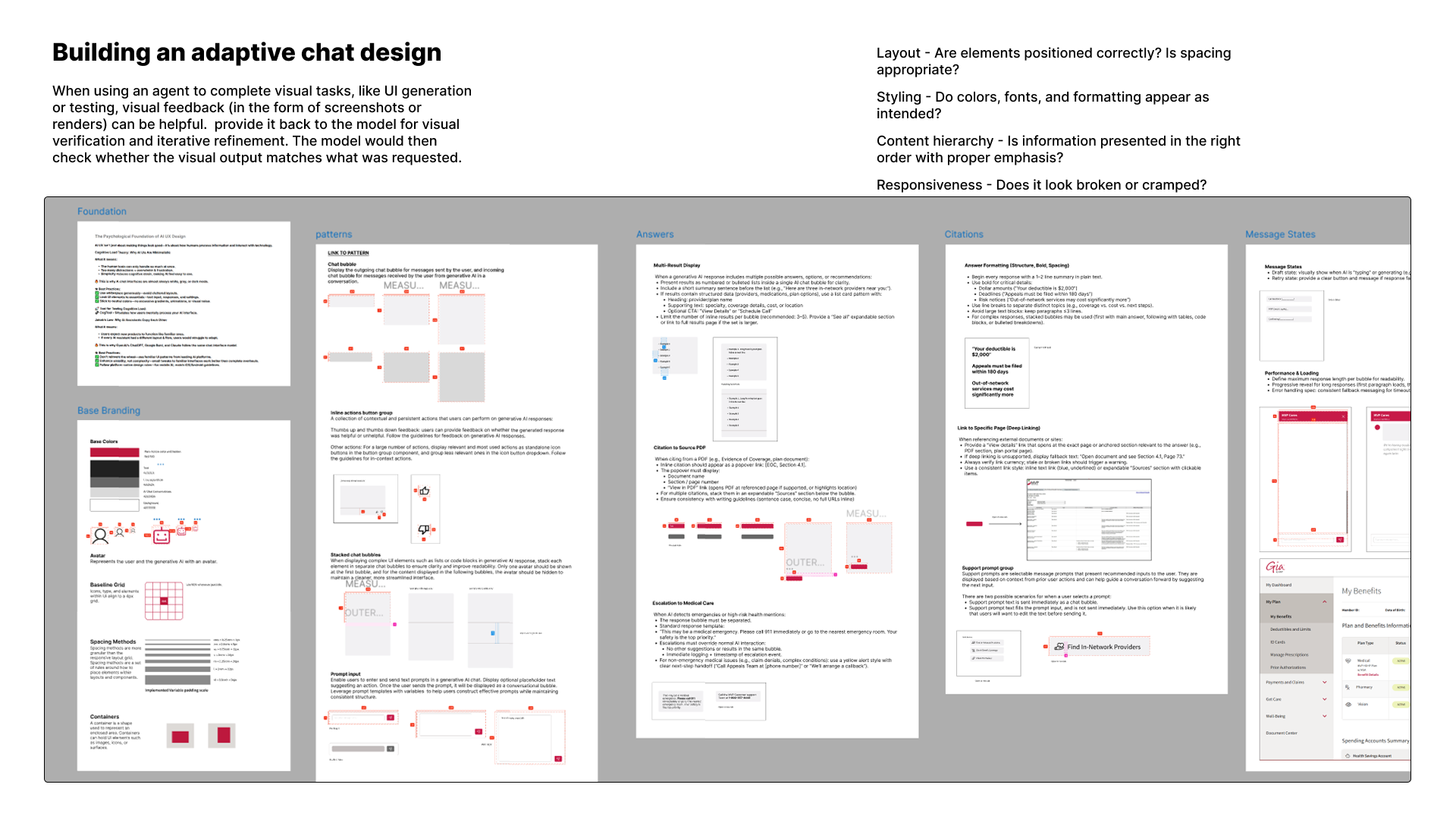
Collaborated with other designer to define visual annotations eg. “presentation rules” for displaying coverage answers, citations, and escalation options. Partnered cross-functionally to create a backlog of features
Result
Team provided engineers with a ready-to-implement design system with UI rules to add to Google Vertex Agent (text, list, CTA, alert, table, link out, etc.) to match content
Deliver
Objective
Helped build and present deck for VP level leadership audience
Contribution
Co-presented problem statement, research, UX guidelines and sample responses.
Result
Launched on 1/26 a prototype AI to the 1500+ MVP employees for testing and feedback.
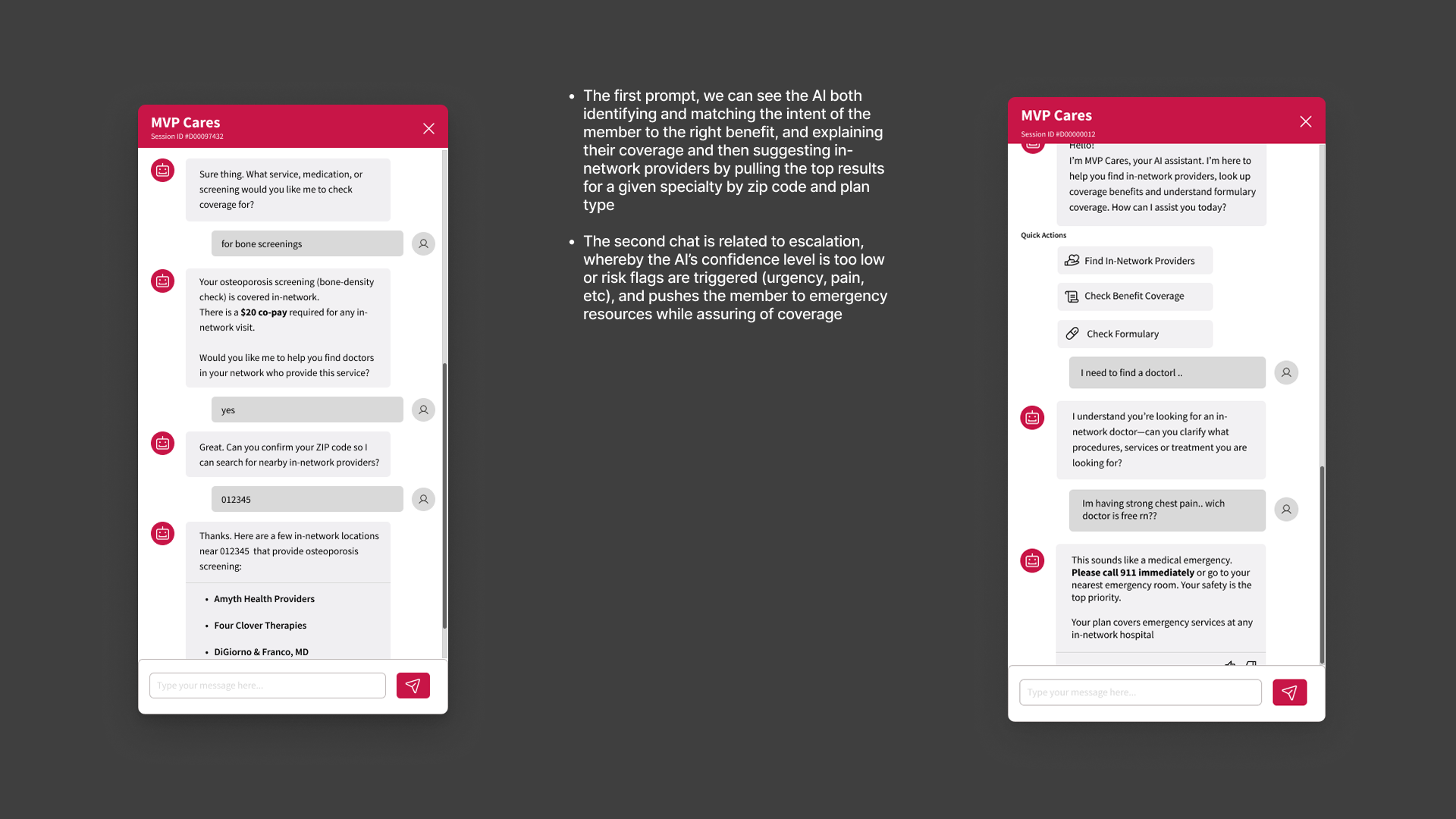
- The first prompt, the AI identifies and matches the intent to the right benefit, and explaining their coverage
- The 2nd chat is shows escalation, whereby the AI’s confidence level is too low or risk flags are triggered, and pushes the member to emergency resources
- The last response attempts to answer ambiguous questions through clarification and validation
.svg)